This article is the first in a series of posts about the importance of understanding physiology when developing medical simulation experiences that will published over the next year. Some simulation team members may have a limited background in physiology or medicine. An understanding of basic physiological concepts can enable non medical simulationists to better understand medical simulation. Physiology is defined as the study of how the body works. Given that there are trillions of chemical reactions going on in the human body in any moment of time, beginning a discussion on physiology may seem an impossible task. There are however, some general concepts that are helpful in understanding some of the basics. (Note: See the entire series linked at the bottom of this article).
Begin by thinking of the human body as a very complex system such as a manufacturing plant. Raw materials, preformed components and gases enter the plant and are assembled into a product that is exported. Fuel is needed to run the plant along with water. Waste products must be eliminated. The human body is no different except the body’s product is chemical, mechanical and transportation work. The body operates in a dynamic state but within defined limits. This is the concept of homeostasis. The body is constantly responding to a myriad of signals/stressors from within and without the body. We are mostly unaware of the majority of these responses except on occasion when for example, we have completed a vigorous exercise activity and respiratory rate and heart rate increases.
Now suppose the body is unable to maintain the steady state. The body may adapt to operating at different level of functionality such as an inability to exercise or eat certain foods or if the stressors are severe enough, the body will stop working altogether. Pathophysiology is the physiology of abnormal states. The human body sends out signals in the well state and when stressed. Heart rate, blood pressure, respiratory rate and temperature (the vital signs) provide minute by minute information about how a person is responding to a stressor in any given situation. Gas levels, labs, urine output, diagnostic tests and subjective statements by a patient provide valuable clues to the clinician about diagnosis and response to treatment. Simulation should mimic real life as much as possible and therefore should include as many components as would typically be found in the corresponding real life situation.
Blood Pressure:
- Blood pressure is a key vital sign which provides information about the body’s ability to move blood around the body.
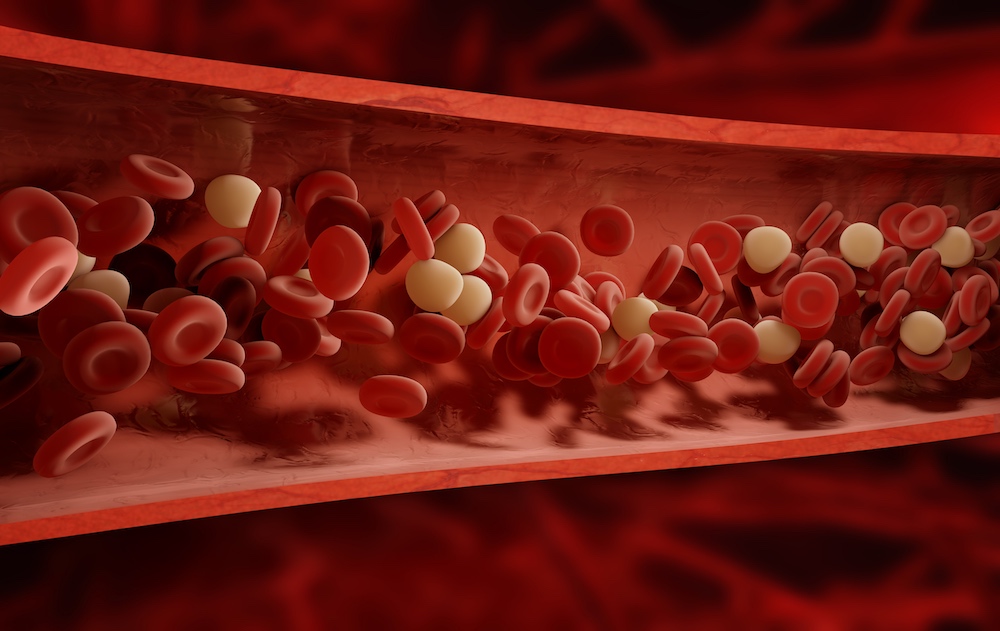
- Blood carries vital oxygen, nutrients and hormones (chemical messengers) as well as waste products to be eliminated via the kidneys, liver and lungs.
- Blood travels in two circuits:
- From the right side of the heart to the lungs and then back to the left side of the heart (blood takes up oxygen and eliminates carbon dioxide).
- From the left side of the heart to the systemic circulation (everything else except the lungs) and then back to the right side of the heart (blood gives up its oxygen and collects waste products).
- The heart has two separate pumps, the left and the right which under normal circumstances do not communicate.
- Blood flows in response to a pressure gradient just like the wind in the earth’s weather system.
- Blood flows from a high pressure area to a low pressure area.
- As the heart wall contracts (systole), the pressure inside the heart chambers increases. This in turn causes the heart valves to open and blood flows out of the heart along the blood vessels in the form of a pressure wave.
- We can feel this wave in certain areas of the body for example the carotid, femoral and radial pulses.
- The bigger the pressure gradient, the bigger the flow.
- When the heart is at rest, it is said to be in diastole.
- As blood flows around the systemic circulation the pressure gradually drops.
- The pressure is lowest in the veins. Valves are needed to prevent blood pooling and flowing backwards.
- Aortic Pressure example:
- Systole e.g. 120 mmHg. Diastole 80 mm Hg
- Pulse Pressure: Systolic pressure – Diastolic Pressure (120-80 = 40 mm Hg).
- Mean Arterial Pressure (MAP): is an average blood pressure in an individual during a single cardiac cycle.
- MAP = 1/3 (SBP – DBP) + DBP (As heart rate increases, the calculation changes since the heart spends less time in diastole).
- Venous return: Lowest pressure in veins. Blood returns to heart by muscle pump, respiratory pump and valves that ensure one way flow.
- Blood pressure is dependent on two major factors:
- Blood Pressure = Cardiac Output (CO) x Systemic Vascular Resistance (SVR)
- The nervous system can have a significant effect on blood pressure:
- The sympathetic nervous increases heart and cardiac output and therefore blood pressure. Think flight or fight response.
- The parasympathetic tends to lower blood pressure. Think rest and digest.
- Resistance:
- The heart pumps against the resistance of the systemic circulation
- The higher the resistance the less the flow
- The lower the resistance the greater the flow.
- Resistance is proportional to:
- Length of blood vessels.
- This is usually a constant number however for every pound of body fat adds approximately 7 miles of blood vessels!
- As body weight increases, the heart has to work harder to overcome resistance.
- Viscosity
- Usually fairly constant but in diseases like polycythemia, viscosity increases and the workload of the heart increases.
- Radius of Blood Vessel
- Vasoconstriction → narrower blood vessel → greater the resistance → less flow
- This is key to understanding blood pressure and hypertension.
- Small changes in radius can have significant effects on blood pressure.
- Length of blood vessels.
- The heart pumps against the resistance of the systemic circulation
- Medications can change blood pressure:
- Vasopressors – increase blood pressure e.g. dopamine, adrenaline
- Vasodilators – decrease blood pressure e.g. nipride, beta blockers, ACE inhibitors etc.
- Cardiac Output.
- Blood pressure is also a function of how much fluid is in the circulation
- BP = CO x SVR
- CO = Heart Rate (HR) x Stroke Volume (SV)
- Stroke volume = amount of blood pumped by one beat of the ventricle during a single contraction.
- The faster the heart beats, the higher the cardiac output, the higher blood pressure.
- Alternatively, when heart rate drops to 40 beats per minute, if nothing else changes, cardiac output would drop and blood pressure in turn would also drop.
- Since cardiac output depends on the volume of circulating fluid
- When there is a sudden drop in blood volume (e.g. in hemorrhage) the body will respond by:
- Increasing heart rate
- Vasoconstriction
- To maintain blood pressure and move blood away from periphery to vital organs.
- These responses may be sufficient to maintain blood pressure however, if blood loss is not replaced, blood pressure will drop.
- When there is a sudden drop in blood volume (e.g. in hemorrhage) the body will respond by:
- Medications can affect fluid levels:
- E.g. Fluids can be replaced → blood pressure will increase.
- Vasopressors.
- Medications that cause fluids to be eliminated via the kidneys.
- Diuretics such as furosemide (Lasix) → fluid volume will drop and blood pressure will also drop.
Subtle changes in vital signs such as blood pressure may give clues to the severity of physiological stressors and how a patient is responding to the stressor. Although this articles focused on blood pressure, vital signs do not usually change in isolation. Blood pressure changes are often key components of simulation. May the force be with you!
Read the Entire Physiology: The “Force” Behind Healthcare Simulation HealthySimulation.com Article Series:
- Part 1: Blood Pressure
- Part 2: Heart & Respiratory Rate
- Part 3: Pulse Oximetry
- Part 4: Diabetes
- Part 4B: Hypoglycemia & Excel Template for Simulated EHR
- Part 4C: Insulin
- Part 5: Sepsis
- Part 6A: Hypovolemia (Intro)
- Part 6B: Hypovolemia (Treatment & Simulation Tips)
- Part 7A: IV Fluids & Bags
- Part 7B: IV Pumps & Site Access
- Part 7C: PCA for Pain
- Part 8: ABGs
- Part 9: Sepsis Labs
Today’s article was guest authored by Kim Baily PhD, MSN, RN, CNE, Simulation Coordinator for Los Angeles Harbor College. Over the past 15 years Kim has developed and implemented several college simulation programs and currently chairs the Southern California Simulation Collaborative.
Have a story to share with the global healthcare simulation community? Submit your simulation news and resources here!