Pediatric simulation scenarios provide clinical educators, learners and professionals with an outline of a pediatric patient case experience to improve performance over time and increase patient safety. Today, Kim Baily of HealthySimulation.com shares the first of two articles intended to offer a pediatric simulation scenario focused specifically on asthma. This article includes an extensive downloadable Electronic Health Record (EHR) with a prescriber order sheet and MAR. Part 2 of this series Pediatric Asthma Scenario Part II + Downloadable Scenario Guide includes a scenario equipment list, scenario instructions and suggestions for expanding the scenario.
According to the World Health Organization, approximately 300 million people in the world (4.3%) have asthma, and 14% of children suffer from the disease. In the U.S., the prevalence of asthma in children has increased 160% since 1980, and the disease currently affects nearly 5 million children. Asthma is the most common chronic respiratory disease in children.
Current treatment options revolve around preventive measures which include regular assessment and monitoring, control of factors that contribute to or aggravate symptoms, pharmacologic therapy, and education of children and their caregivers. The National Asthma Education and Prevention Program guidelines recommend a “stepwise approach to pharmacologic treatment, starting with aggressive therapy to achieve control and followed by a ‘step down’ to the minimal therapy that will maintain control.”
In spite of these preventive measures, every year in the U.S. there are 500,000 hospitalizations due to asthma, 44% of which are children. Clinical staff need to assess asthmatic patients and intervene quickly, since these patients can often rapidly deteriorate.
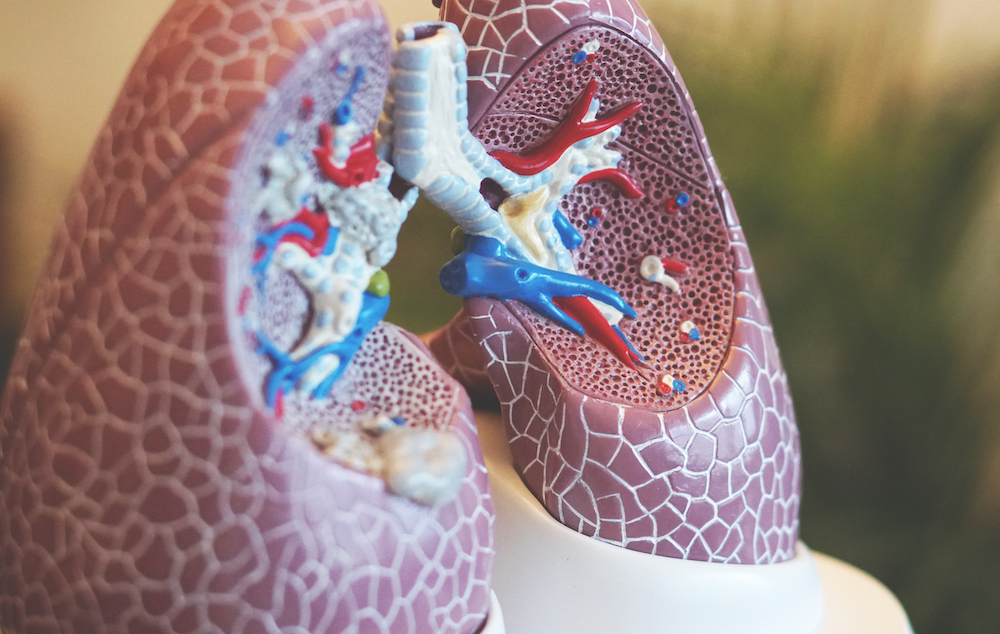
Asthma is a heterogeneous disorder in children that is characterized by recurrent airway obstruction, bronchial hyper-responsiveness and airway inflammation. Reactive airway disease (RAD), or reactive airways dysfunction syndrome (RADS), is a nonspecific term often used interchangeably with asthma. RAD is most often used as a “catchall” diagnosis for children who may or may not have asthma, and is a term that has limited clinical significance (Malo, Chan-Yeung, & Lemiere, 2014).
Pathophysiology: Inflammation in the airways causes increased mucus production, swelling of the mucosa and contraction of the muscles of the airway. These changes diminish the effectiveness of the airway and cause chest tightness, coughing and wheezing, especially at night and in the early morning. Children have a different anatomy which affects the way asthma manifests itself. Infants have smaller nares, and are obligate nose breathers until about 1-2 months of age. Children 8 and younger have immature cartilage, and the epiglottis is more flaccid, making it difficult to completely close.
A child’s trachea has a narrower diameter than an adult’s. Lung tissue develops and grows from birth to about the age of 12. The alveoli multiply over 10 times the amount an infant is born with. Children younger than 6 breathe with their abdominal muscles, as there is weak musculature with thoracic muscles. According to the American Lung Association, triggers for asthma include exercise, allergies, infection, pollutants (including secondhand smoke), changes in the weather, emotional stress, sudden temperature changes and diet.
Signs and Symptoms: Asthma is characterized by variable and recurring symptoms, including wheezing; coughing (which can be irritating and nonproductive); chest tightness; shortness of breath; difficulty breathing, especially at night and early in the morning; tachypnea; retractions and/or nasal flaring; and hypoxia and cyanosis with severe attacks.
Other Diagnostics: Spirometry, lung volumes, infant pulmonary function testing, methacholine challenge, bronchoscopy and laryngoscopy.
Medications:
- Short-acting beta2-agonist (bronchodilator): Used for quick-relief/rescue medication, such as albuterol, which is administered by nebulizer or MDI/spacer. (1.25 mg in 3 ml via HHN every 4 hours).
- Inhaled corticosteroids are the most effective medications for long-term management of persistent asthma, and should be utilized by patients and clinicians as recommended in the guidelines for control of asthma. Corticosteroids act by reducing swelling and mucus production in the airways. As a result, airways are less sensitive and less likely to react to triggers. For example, budesonide (Pulmicort): children 12 months to 8 years of age — 0.5 to 1 milligram (mg) in a nebulizer once a day, or divided and given twice a day. Methylprednisolone (Solumedrol) 1-2 mg/kg/day in 2 divided doses.
- Leukotriene Modifiers (LM): Leukotrienes stimulate smooth muscle hypertrophy, mucus hypersecretion and the influx of eosinophils into airway tissues, LMs block these effects, e.g. montelukast (Singulair) chewable tablet 5 mg PO daily.
Notes on Excel EHR
The Medication Administration record has “if” statements written into the patient and medication pages. The patient’s ID (bar code) can be scanned into the blue scan boxes. To the right of each blue cell is a hidden statement that will show “correct ID/med” if the scanned bar code matches, or “error check ID or med” if the bar code does not match. If the blue cell is empty, nothing is shown. If you are not scanning ID or meds, this option can be ignored. Avery offers free bar code scanning software for printing on labels.
Nursing diagnoses appropriate for an asthma patient include ineffective airway clearance, ineffective breathing pattern, anxiety and ineffective therapeutic regimen management. The type of scenario developed for a pediatric asthma case study will depend on the learners participating in the simulation.
Prebriefing information provided to the learners ahead of the simulation day will also vary depending on the learner and the stated learning objectives. Providing learners with a brief outline of the clinical case, list of medications, study guide or clinical references to standards of care and treatment may be helpful. The second part of this article Pediatric Asthma Scenario Part II + Downloadable Scenario Guide includes scenario details and equipment lists.
Download the Pediatric Asthma Pneumonia EHR here!