Oxford Medical Simulation (OMS) develops true to life virtual reality healthcare simulation scenarios, with full feedback and debrief capabilities, to allow VR to do the work, so sim labs can be more efficient and effective in their educational and training process. OMS has designed their VR simulation system to be seamlessly embedded into any university or hospital simulation center or skills lab. With complete libraries of scenario content for RN, ANP, nursing student, medical student, resident, behavioral health, and community health, your program can get the ground running with VR training with Oxford Medical Simulation. Today we take a closer look at their training platform to see where the future of simulation in healthcare is going with Virtual Reality! Attending INACSL this week in Phoenix, stop by and check out OMS at Booth #101!
What is Virtual Reality Simulated Training Anyway?
Virtual reality (VR) is a technology where learners are immersed in simulated environments and are able to engage and interact in a way that feels real. VR has the unique capability – more so than any technology that has ever existed – to let users suspend their disbelief and learn from experience in the same way as real life.
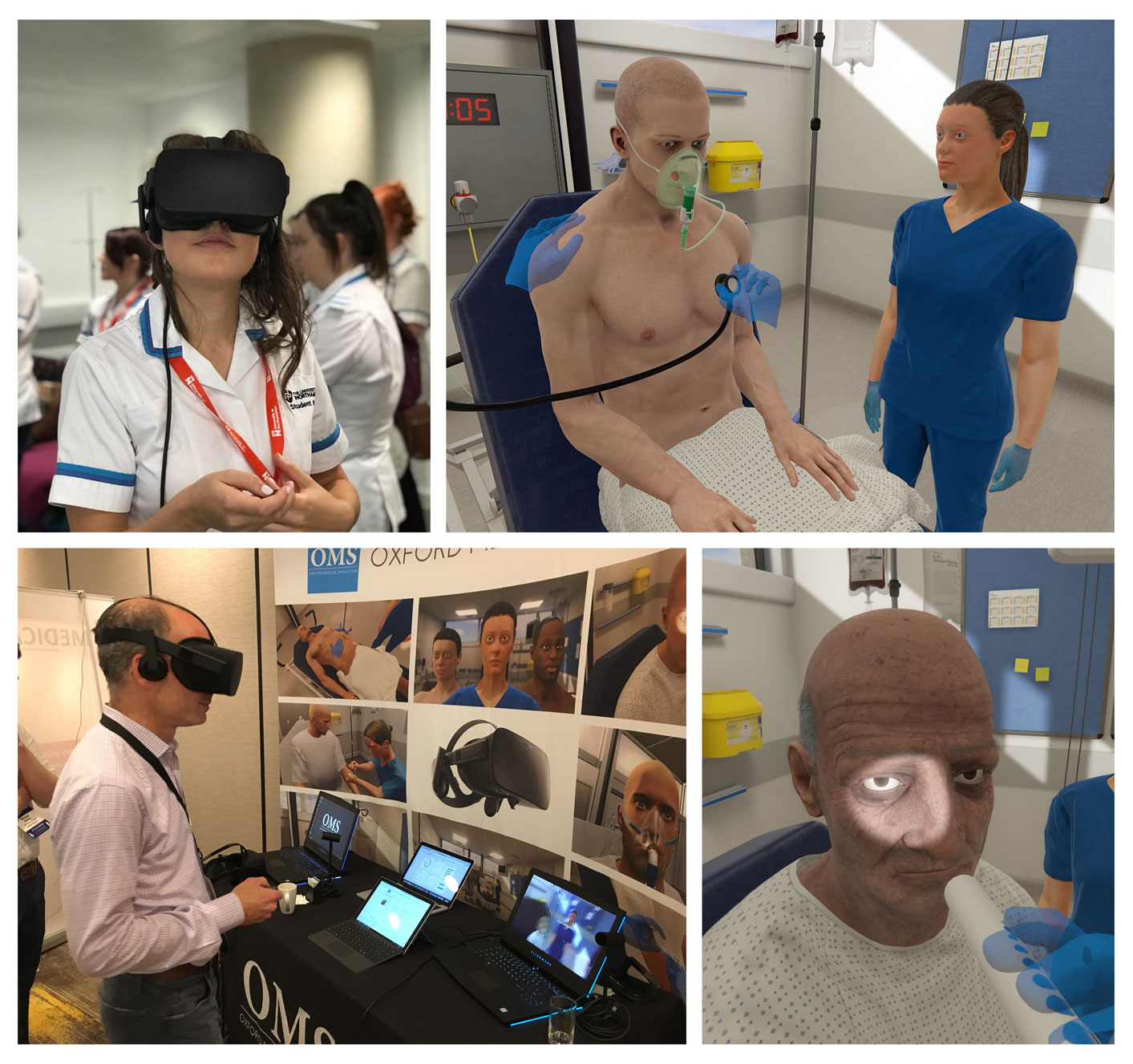
In putting on a VR headset, users cognitively enter a new world, and if that virtual world is an ED, with patients, monitors, relatives, alarms then learners will behave like they do in real life. OMS is harnessing the power to deliver clinical simulation at a global scale.
How Does OMS VR Work?
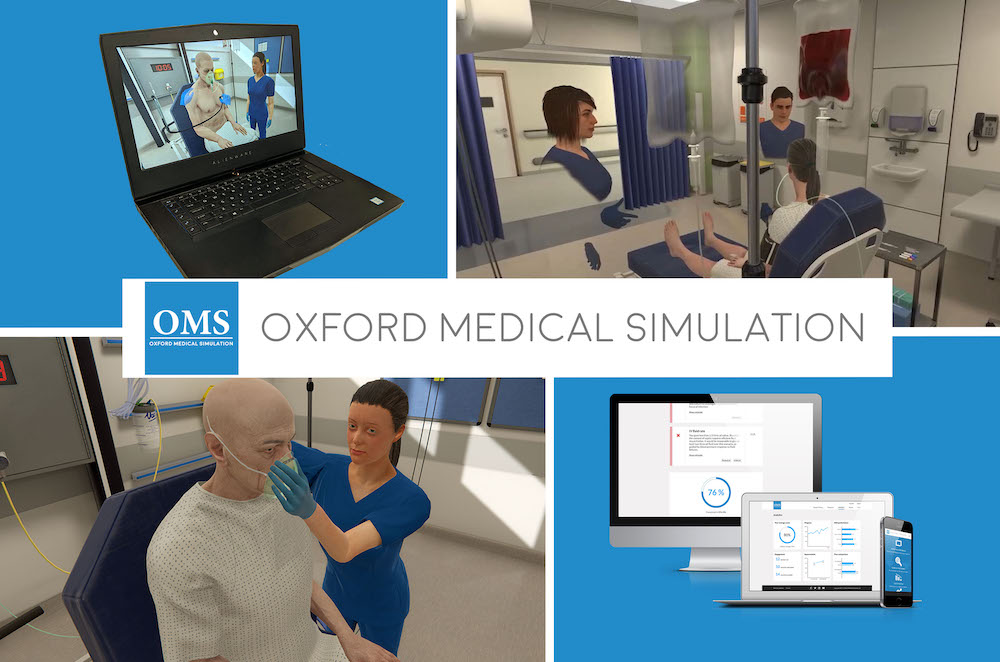
Using Oculus Rift S VR headsets, high fidelity simulation learners enter into immersive emergency scenarios and meet patients whom they must manage as they would in real life. The scenarios, written by OMS’s team of clinicians and educators with learning customizable by each institution, focus on decision-making, clinical reasoning and critical thinking. Learners can do everything they would be able to do in physical simulation, from taking a full medical history, performing physical examinations, ordering and interpreting investigations, liaising with colleagues, managing your team and prescribing medication.
Everything works as in real life. Conversation is dynamic and adaptive, as are patient vitals and results – adapting to learner actions and treatments. Protocols are built in, as is radiology, EKGs, fluid charts and an EMR. Relatives, colleagues and the interdisciplinary team must be managed as in real life, with a focus on both the technical and the non-technical skills. Once the scenario is completed the learner is guided through a period of self-reflection to allow them to explore what they learned and how it applies to their practice.
Every action the learner takes during the scenario is logged and analyzed against best practice. Once the guided reflection is complete the learner is presented with their results. Feedback is tailored to meet institutional guidelines and takes the learner through what they did well and what they could improve on. The feedback personal, adaptive and linked out to institutionally specific blended learning – allowing VR to become a hub for learning.
This not only gives learners an opportunity to explore strengths and areas for improvement in technical skills, but also non-technical skills. The OMS system looks in detail at task allocation, prioritization, time management and communication with team and patient – to give a holistic summary of performance for the learner to review and improve on. Learners are also given a score to help track progress over time.
Debrief in VR or Back in The Real World
Faculty then have two options. They can either do a physical debrief using the feedback as prompts for debriefing – allowing asynchronous debrief and performance review – or lead the learner self-debrief where the whole system runs faculty free!
As well as making medical simulation more flexible and scalable, the insights from the individual learner feedback are collated into detailed data and analytics reports. Faculties and institution leadership can use this data to assess how learners are performing, which areas need more attention, compare across cohorts and prove ROI.
As virtual scenarios can run 24/7 and be repeated as often as needed, at consistent standardized quality, OMS allows sim centers to increase their throughput, save money and save time – whilst building learner confidence and competence.
Who Should Be Considering VR Now?
Oxford Medical Simulation has designed this VR simulation system to be seamlessly embedded into any university or hospital simulation center or skills lab. They have libraries for RN, ANP, nursing student, medical student, resident and increasingly behavioral health and community content. With over 50 scenarios and content growing every month – whole curricula can be covered. All patients have full histories and personalities, and often have multiple comorbidities to keep you on your toes.
Institutions across the world are already using this innovative platform to transform their healthcare training. This includes hospitals, universities and simulation centers across Massachusetts, New York (including New York University and NYU Meyers College of Nursing) and global clients including Oxford University, Cambridge University Hospital, University College London, Northampton University and the UK’s National Health Service (NHS).
How Others Are Using OMS for Training, Assessment and Recruitment
At the University of Northampton the OMS system has been integrated within the wider skills lab to complement existing resources and service the nursing school at scale. Virtual reality scenarios sit alongside traditional manikins in the simulated ward to provide opportunities for blended learning. Nursing students are able to practice physical procedures using mannikins whilst honing their clinical reasoning and decision making in the virtual scenarios. The University described how, “since nursing is a complex and challenging profession which encompasses a range of skills including people skills, soft skills and clinical skills, we needed to be able to train future nurses in a balanced way that caters to each of these skill sets. The OMS system allows us to integrate theory into practice in a really meaningful manner, allowing progression throughout their academic career.”
Furthermore, Health Education England has rolled out the technology across 18 NHS hospitals to systematically change simulation based training.
Dr. Jack Pottle, Founder and Medical Director of OMS, shared that “Our vision for OMS is to enhance patient care by transforming healthcare training with immersive technologies. Working with Health Education England is great validation for that vision – demonstrating how OMS technology can be used across national health systems to bring about innovation and improved patient care.”
The Research Supports the Effectiveness of Cost-Saving VR Simulations
The OMS system has been through independent trials to demonstrate its impact on learning and performance improvement. More widely, academic papers have demonstrated similar results. In an excellent 2018 paper Haerling demonstrated that VR simulation can be just as effective as physical simulation in achieving educational outcomes whilst being more cost effective. This research has built on twenty years of VR research demonstrating VR’s superiority over screen-based learning (e.g. Gutierrez, 2007) VR’s acceptability and usability (e.g. Harrington, 2017) and VR’s impact on performance (e.g. Maytin, 2015). In fact, as VR simulation has been in use in the aviation and military fields for the last 20 years, and surgery for ten years, it is only surprising it hasn’t caught on in medical and nursing fields more quickly.
Those attending INACSL 2019 this week in Phoenix should stop by and check out OMS at Booth #101 — tell them HealthySim sent you!