During COVID-19, nursing simulation faculty and staff quickly realized that virtual reality in simulation is where the industry’s future is headed. As many nursing programs scrambled to find suitable clinical replacements, virtual simulation presented a method of learning that met pandemic safety requirements and protocols. Since this pivotal shift in healthcare education, both learners and educators have experienced the benefits of virtual simulation. Many found new, creative ways to use virtual simulation to enhance nursing curricula and learning outcomes. This article discusses emerging ideas on the uses of virtual simulations, as presented during a May 2021 HealthySimulation.com webinar.
According to Dr. Laura Gonzalez, Ph.D., APRN, CNE, CHSE-A, ANEF, FAAN, vice president of clinical learning resources at Sentinel U, the most obvious reason to use virtual simulators is to deliver content in a remote asynchronous environment. Virtual simulation in healthcare allows learners to move at their own pace, presenting an attractive concept in competency-based programs.
Gonzalez explains that this is critical as the simulation community begins to adopt and understand how the new AACN Essentials (2021) impacts pre-licensure or entry-level professional nursing education. Like manikin simulation, she explains that virtual simulation offers the ability to experience high-risk, low-volume situations. Additionally, virtual sims provide a psychologically safe environment and the opportunity to “do it again.”
“I could choose the wrong path now, and then I’ll go back, repeat it, and I’m going to correct it. I’m going to choose the correct path, and I can see the difference, and that’s that ability to critically think,” Gonzalez said. “Then, of course, you want to have that formative assessment, the ability for the scorecard to be available for both the learner and for the faculty to make some assessments.”
She added that the theoretical framework of virtual simulation is also valuable when talking about virtual simulation as deliberate practice. Virtual simulations are based on the theory of deliberate practice and engages learners with an opportunity to continually repeat actions to achieve mastery. Gonzalez noted that current literature supports that simulation-based education is effective and achieves such clinical goals.
“We can’t give every learner 25 hours of high-fidelity primary learner experience in a clinical and their normal neuro nursing clinical educational program, but we can provide them with 25 hours of digital access,” Gonzalez said. “I think this pyramid is gaining this whole new level of virtual digital patients and other kinds of ways to provide for this expanded democratized approach, which enables for a further kind of understanding of the content without the physical need to be in a location.”
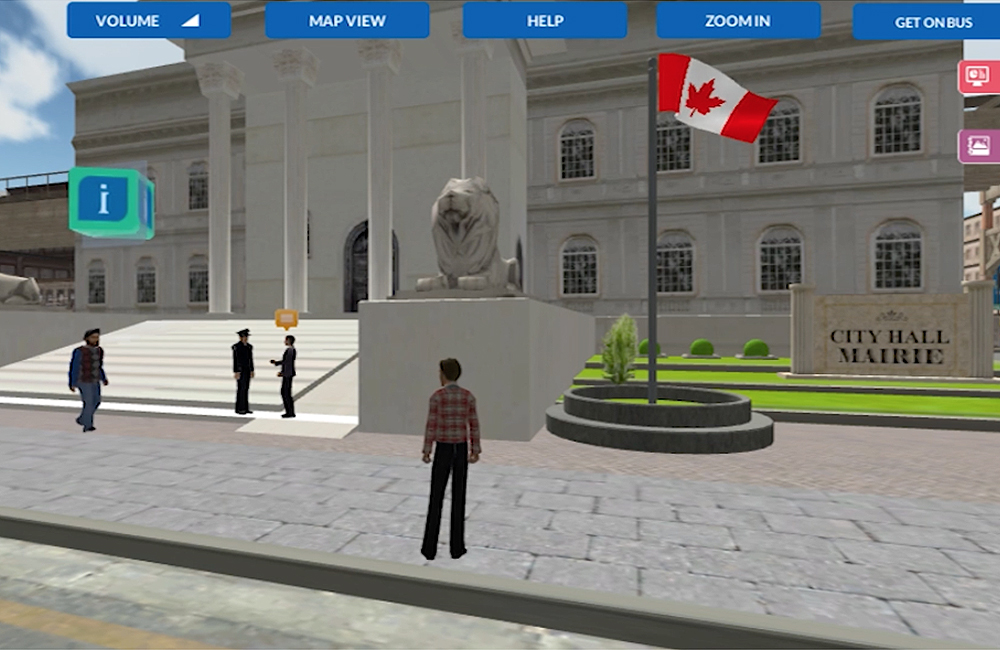
Therefore, simulationists must consider how digital technologies can add and complement clinical simulations, not replace them, but augment them. Yet, they must also consider how and when virtual simulations most appropriately fit into a nursing curriculum. Overall, the opportunity to be in an environment where the learner can think like a nurse or make real world decisions like a nurse can easily occur in a virtual environment, Gonzalez notes.
“We can use virtual simulations as a preclinical activity. If I know my students are going to a neuro ICU, or maybe in advance of going, (I would) perhaps not (be) assigning a didactic chapter from their very large med surg(ical) book, but rather have them complete particular virtual sims in advance of the pre-simulation activity,” Gonzalez said.
According to Gonzalez, this is an ideal alternative because virtual clinical simulation allows both practicing nurses and nursing students to sharpen their communication, collaboration and leadership skills. In addition, virtual simulation can be used as a checkpoint to gauge the pulse of a learner, which is a very viable resource because of potential objectivity. Proving the effectiveness of VR learning, the NCSBN worked to put together a landmark study that demonstrated that up to 50% of clinical time could be replaced with simulation without adverse effects.
“I think we have just begun to see the evolution of virtual simulation. I also think we’re going to see a lot more of it in our curricula as curricular replacements continue,” Gonzalez concluded. “I don’t think we should think of a virtual simulation as something we did during the pandemic, that we don’t need to do anymore. It is more than that. It has a place in our curriculum, and I think we need to be thinking in those terms.”
Putting virtual simulation into practice, Sentinel U is an e-learning company that works to meet the evolving needs of healthcare education and training by providing simulation-based technologies and virtual learning tools. Founded in 2013, Sentinel U helps advance nursing academic education and healthcare professional training through virtual clinicals that are engaging, effective and economic. Aligning outcomes with AACN BSN Essentials, QSEN Competencies and NCLEX categories, Sentinel U provides nursing learners and practicing nurses with online simulations that are convenient to safely practice healthcare and patient scenarios anywhere, at any time, while earning virtual clinical hours.
More About Dr. Laura Gonzalez
Dr. Gonzalez is an internationally recognized simulation expert. She is one of 76 advanced certified healthcare simulation educators (CHSE-A) globally. In the fall of 2020, she was recognized by the prestigious American Academy of Nurses as a Fellow (FAAN). She is the 2021 President-Elect for INACSL. She is also a fellow of the Academy of Nurse Educators (ANEF).
Her professional nursing and academic career is focused on advancing the science of nursing education through the use of simulation and its impact on learner outcomes. She has a very specific body of work that has resulted in over 20 data-based manuscripts in peer-reviewed journals, and one clinical skills textbook. She was Co-PI on a large interprofessional grant through the National Science Foundation (NSF). Her team was able to demonstrate that learners were more engaged and had a higher sense of urgency when interacting with an augmented virtual reality simulator.
Her article on deliberate practice reached a readership milestone. She is one of several scientists to have two patents: on Detecting Sterile Field Events and Related Methods and Virtual Patients. Lastly, she is a nurse educator with vast experience teaching across the curriculum to include live, hybrid, online and synchronous delivery methods.