Fidelity in healthcare simulation is a key factor in the creatioProfessional Developmenn of meaningful educational experiences. When learners pretend to wash hands or operate IV pumps during simulation scenarios, the realism of the experience is interrupted and the learner loses focus on the scenario learning objectives. This article reviews various types of infusion pumps and how they are operated and programed. This is part 7B of our ongoing series by Dr. Kim Baily on Physiology: The Force Behind Healthcare Simulation – A Guide for Techs. See the complete series linked below!
An infusion pump is a medical device that delivers fluids, such as nutrients and medications, into a patient’s body in controlled amounts. There are many types of infusion pumps, including large volume, patient-controlled analgesia (PCA), elastomeric, syringe, enteral, and insulin pumps. Other devices include fluid warmers and rapid infusion devices typically used for blood and other fluids in critically ill patients. Infusion devices are used extensively in hospitals, nursing homes and in the home. Some are portable and may be worn by the user as they move about.
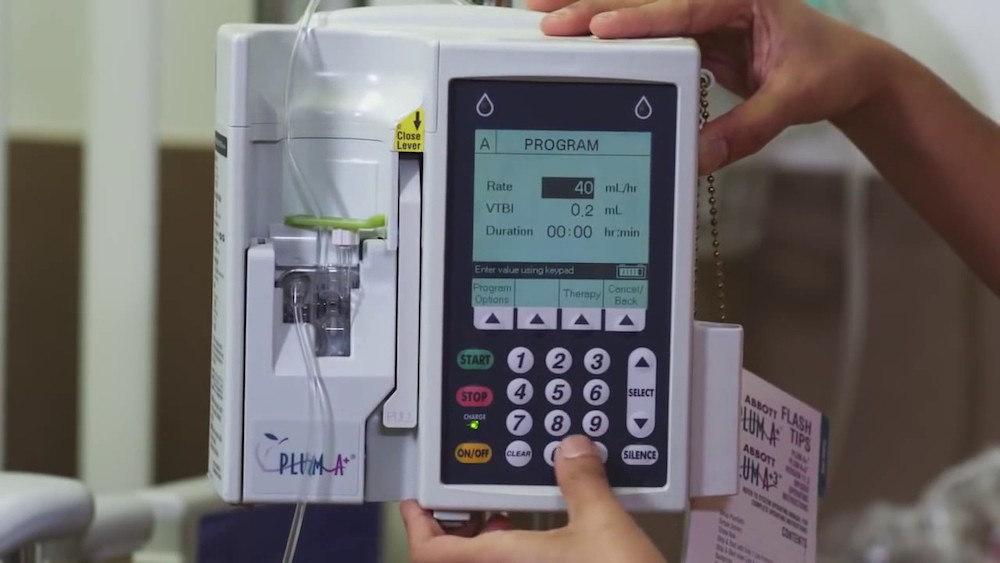
Below is a closer examination of IV Pumps and how they can be incorporated into medical simulation.
IV Pumps and Operation
- The advantages of infusion pumps is their ability to accurately deliver and measure infusion volumes and to infuse the volumes at controlled rates. Pumps provide pressure to overcome resistance to ensure a steady flow. Many so called “smart pumps” can calculate doses and can warn operators of errors.
- When a pump and system is working with normal resistance, delivery pressure is minimal. When resistance (5 psi over baseline) develops in the catheter or tubing, the pump adds pressure (within limits) to maintain infusion. Changes in resistance at an insertion site due to infiltration or thrombosis may not set off the system’s alarm. When the pumps maximum pressure limit is reached, an occlusion pressure alarm sounds. Some pumps can distinguish between upstream pressure (e.g. closed roller clamp on tubing above pump) or downstream pressure (blocked IV access).
- Smart Pumps: Some pumps connect via wifi to electronic health records, pharmacies or to healthcare practitioners to warn them of incorrect dosing or empty fluid bags.
- When pump settings do not match facility’s drug administration guidelines, pump will alarm.
- Data may be logged from pump to pharmacy database. Data may include time, date, drug that was infused, concentration, programmed rate and volume infused.
- Information from pharmacy can be programmed into the pump.
- Facilities program pumps with specific data sets or “profiles”. Each area of the facility develops their own drug library, i.e. OB, peds, ICU etc.
- Barcode information attached to IV bags can be wirelessly transmitted to pharmacy – pump will not infuse if scanning incomplete.
- Additional features include: add on syringe pumps for small volume infusions, multiple pump infusions from one machine and patient controlled analgesia.
- Syringe Pumps
- For small volumes
- Uses microbore tubing.
- Prefilled syringes attach to pump.
- Patient Controlled Analgesia (PCA).
- Specialized pumps that allow patients to control the amount of analgesia they receive – See Physiology – The Force Behind Simulation Part 9. PCA.
- When several pumps are needed, individual pumps may be attached to a pole or a unit consisting of several pumps joined together may be used (multi-infusion pumps). These pumps are more common is critical care areas where multiple infusions may be ordered. Each pump operated independently.
- The main IV fluid running is designated as the primary line or maintenance IV. The primary IV may run continuously or before and after medication administration. The use and volume of maintenance IVs depends on the fluid status of the patient.
- Most pumps use tubing specifically designed for the pump (aka administration sets). Tubing is often primed (filled with fluid) before placing in pump.
- Tubing should never be primed when the IV is attached to patient – air may enter the body.
- Smart pumps can prime and back prime (secondary bags can be filled from primary automatically).
- When a medication is needed such as an antibiotic, the medication is often prepared by pharmacy and is sent to the nursing station in a separate bag – aka secondary bag or piggyback.
- If the pump only has one channel, the medication bag is piggybacked ABOVE the pump. The bag which is highest will run first i.e. when the piggyback is hung above the primary and the roller clamp on the piggyback tubing is OPEN, the pump will drawer fluid from the piggyback first (due to gravity). When the piggyback empties and the fluid level within the piggyback tubing levels with fluid in the primary bag, fluid will leave the primary bag.
- Learners often have difficulty understanding gravity versus pump infusions. Simulation makes an excellent way for learners to become skilled.
- Two different rates and volume are set for the primary fluid and the secondary (piggyback).
- E.g. primary rate – 100 mL/h. VTBI 1000mL.
- Secondary rate – 200mL/h. VTBI 50 mL.
- 50mL secondary (piggyback) will empty in 15 minutes.
- With a single channel pump, the rate automatically converts back to the primary rate after 15 minutes.
- NOTE: If the operator forgets to open the roller clamp on the secondary bag, the pump draws 50mL from the primary line instead. The pump cannot tell which bag is providing fluid.
- This is a common error. Patients either do not receive the medication in the secondary bag or the medication is given late.
- Two different rates and volume are set for the primary fluid and the secondary (piggyback).
- Smart pumps have built in features to prevent the above error. They have a secondary channel for IV piggybacks. When the piggyback volume, flow rate and start control are set, the pump will alarm if no fluid leaves the secondary bag.
- No pump infusions aka gravity infusion:
- All IV tubes have a drip chamber at the top of the tubing which allows the operator to see that fluid is flowing.
- When pumps are not available, IV tubing is connected directly from the IV bag (hung on a pole above the patient) and drops per minute are counted in the drip chamber to estimate flow rate. The size of the opening within the drip chamber determines the drop rate – the larger the opening, the larger the drop and the smaller number of drops are needed to make up one mL.
- Tubing is labeled with the drop rate e.g. #10 means 10 drops are needed to make 1 mL, #60, 60 drops are needed to make 1 mL (aka microdrip).
- Piggybacks operate by gravity and must be higher than the primary IV bag. The operator must calculate a new drip rate for the piggyback and close the primary. When the infusion is finished, the secondary is closed and the primary opened and the primary drip rate confirmed.
IV Dosage Calculations
- Flow rate mL/hour:
- Common calculation for IV pump.
- Total Solution/No. of hours to run = mL/hour
- E.g. 1000 mL to run over 8 hours = 125 mL/hour.
- Micrograms/kg/minute:
- Medications such as dopamine have different effects at various infusion rates.
- To increase renal perfusion, dopamine is run at 2 mcg per kg per minute. Weight and medication concentration within an IV bag can be programed into a smart pump which will automatically calculate the flow rate.
- E.g. 100 kg person (Learners should calculation method used at institution).
- 2 mcg x 100kg = dose per minute for this patient = 200 mcg dopamine per minute (200 mcg x 60 per hour).
- Concentration of dopamine bag = 400mg dopamine /500 mL = 800 mcg/mL
- Flow rate mL / hour = (200 x 60) / 800) = 15 mL/hour.
- Medications such as dopamine have different effects at various infusion rates.
- Drops per minute
- Method used when no pump is available.
- mL/h x drop factor/60 minutes = drops (gtts/minute)
- E.g. 100 mL/h = (100 x 10) /60 = 16.67 gtts/minute (often rounded to 17 gtts/min).
- The operator must count drops in 60 seconds and adjust to correct rate.
- This is much less accurate than using a pump since:
- Flow may change as the patient moves.
- The higher the bag, the faster the infusion rate.
- Increased blood pressure or coughing may slow the infusion rate.
- If the tube becomes blocked or the IV bag becomes empty there is no alarm to warn operator.
Safety Tips for IV Pumps
- The FDA monitors safety issues associated with infusion pumps which include over or under infusion and missed or delayed treatment. Errors may be due to operator error or to pump failure. From time to time pumps are recalled.
- Pumps and IV infusions are closed systems. Maintaining sterility is critical. Contamination of pumps or IV tubing can introduce microorganisms into the bloodstream, which in turn can lead to sepsis. Connecting tubing should follow strict hospital protocols to prevent contamination.
- IV tubing should be free from damage such as cuts, kinks, or disconnections before and during use, as these can be a source of air in the tubing.
- When multiple pumps are in use consider labels for pumps showing medication.
But how can we use IV Pumps best in Clinical Simulation?
Simulation Variations for Scenarios with Infusion Pumps
- Basic safety/environmental check simulations:
- Most hospitals have labels to attach to broken or malfunctioning equipment. Add a label to the pump at the patient’s bedside. Learners should notice and change pump. This scenario will provide practice in setting up the pump.
- Medication/Fluid Errors.
- Outdated or non-labeled tubing.
- IV fluid belonging to another patient hanging.
- Outdated fluids.
- Wrong IV fluid hanging e.g. 0.9% sodium chloride versus 0.45% sodium chloride.
- Incorrect medication hanging e.g. wrong rate, wrong concentration of medication in IV bag or incorrect medication.
- Infusion rate beyond recommended guidelines e.g. Potassium infusing at 30 mEq/h.
- Blood hanging with 0.45% sodium chloride
- Gravity dependent IV piggyback or single channel pump with piggyback clamp closed (i.e. patient receiving primary IV at secondary rate).
- O715 Shift report: Off-going nurse states that IV piggyback was hung at 0600 but in actuality, the roller clamp was not opened and the patient did not receive medication. The piggyback is hanging full at the bedside.
- This type of scenario can also be used to discuss reporting errors and completing incident reports.
- PCA setting does not match orders. PCA is almost empty and learner must change analgesic syringe and tubing.
- Have patient develop signs and symptoms of air embolism such as a sudden onset of chest pain or tightness, difficulty breathing or shortness of breath, lightheadedness, fainting, or confusion.
- Use Moulage to indicate IV site infection or inflammation.
Intravenous medication administration and the various potential complications and errors associated with IV infusion pumps occur regularly in the clinical setting. Healthcare simulation scenarios create an excellent way to provide practice in clinical skills and to develop problem solving skills.
Further Reading From The Urgent Need for Innovation in I.V. Smart Pumps (Karen K. Giuliano, PhD, RN, FAAN and Charles Niemi, MS, CISSP)
More than a decade ago, the introduction of smart I.V. pumps with drug libraries and dose error reduction systems (DERS) provided a means of reducing I.V. medication infusion errors that hadn’t been previously available. However, even with the availability of smart pumps, errors continue to occur in every clinical setting. A 2005 study found a staggering 67% error rate with the administration of I.V. infusions on an ICU.1 Common sources of error include overriding of dose error alerts and, even more concerning, using basic programming to bypass the smart pump’s drug libraries and DERS completely. We provide an overview of the major I.V. smart pump user issues so that you can be better prepared to facilitate technology innovation in this important area of patient safety.
Because nurses are the primarily users of I.V. infusion devices, nurse leaders are in a key position to promote improvements in this very important area of patient safety. It will take a village of clinical users, pharmacists, human factors experts, and I.V. infusion device manufacturers working together to adequately address the multiple and complex issues associated with improving the ease of use and safety of I.V. medication infusion devices. This process must be combined with a disciplined and ongoing program of clinical outcomes research to generate credible evidence that can stand up to peer review to measure how well we’re progressing. These research findings then need to swiftly make their way into clinical practice. Only then will meaningful and lasting improvements in this important area likely be achieved. Read the full “Urgent Need for Innovation in I.V. Smart Pumps” article.
About the author: Kim Baily PhD, MSN, RN, CNE, is the previous Simulation Coordinator for Los Angeles Harbor College and Director of Nursing for El Camino College. Over the past 16 years Kim has developed and implemented several college simulation programs and previously chaired the Southern California Simulation Collaborative.
Subscribe for More Great Simulation Resources!
Physiology: The “Force” Behind Healthcare Simulation HealthySimulation.com Article Series:
- Part 1: Blood Pressure
- Part 2: Heart & Respiratory Rate
- Part 3: Pulse Oximetry
- Part 4: Diabetes
- Part 4B: Hypoglycemia & Excel Template for Simulated EHR
- Part 4C: Insulin
- Part 5: Sepsis
- Part 6A: Hypovolemia (Intro)
- Part 6B: Hypovolemia (Treatment & Simulation Tips)
- Part 7A: IV Fluids