Healthcare Simulation Educators and Simulation Operation Technicians are tasked with the development of new and creative strategies for solving the need for learners to have experiential opportunities. This calls for simulationists to think outside the box and discover ways to meet the learning outcomes on a limited budget. This HealthySimulation.com article written by Samantha Marie Scaffidi, BSN, RN, is to describe how to make a task trainer port that can be palpated, accessed, and infused.
The Problem Called for a DIY Solution
Yearly the hospital system does multiple in-depth outpatient chemotherapy competencies. This involves interoperability between EPIC charting system and Alaris infusion pumps. The training involves trained chemotherapy nurses to hang, dual verify, and infuse simulated chemotherapy as a part of their yearly training. A majority of the patients receive chemotherapy via a Medi-port. Therefore, the fidelity of the access and infusion in a Medi-port is imperative for this simulation to have a port that can have fluids administered through. This skill cannot be accomplished or demonstrated without the psychomotor skills. A solution to address the issue had to be developed.
Material To Create Port and Drainage System
The simulationists must develop a realistic infusion port that has a drainage system incorporated. The materials required for this task trainer are:
Port:
- 4×4 Silicone suture pad (From Amazon, Suture Practice Fake Skin, Silicone Skin Layers Surgical Skin Injection Practice Pad Suture Training Model)
- 5-0 suture (can use needle and thread)
- Para-film
- Power-port
Drainage system:
- Desired length of IV arm silicone tubing
- 3-way stopcock
- Secondary Tubing
- Empty IV bag
Method
For the port, a double-sided silicone suture pad with a foam center was chosen. This was bought from Amazon. The new suture pad was cut in half via the foam center and then trimmed to about a 4 inch by 4 inch square. The foam was then cored out to fit the donated medi-port and sutured in place. If there is no access to suture material, a needle and thread would work just as well.
To create a drainage system, old IV arm tubing was used to connect to the medi-port’s line. Alternate tubing could be used with considerations for the tubing to surround the port’s line by at least two inches to prevent backflow and the tubing cannot be so large in diameter that a male luer-lock adaptor end could not be placed. Once the silicone IV arm tubing was placed, Para-film was wrapped around the tubing to seal the gaps and prevent leaks.
A 3-way stopcock was attached to the luer-lock end and an Alaris pump secondary line tubing with empty IV bag was attached to the distal end. The top of the stop cock was capped but could be used as a blood supply for return on port access. Do note that if running the port with any clear fluid for a period of time will dilute the blood supply unless “turned off” from the supply.
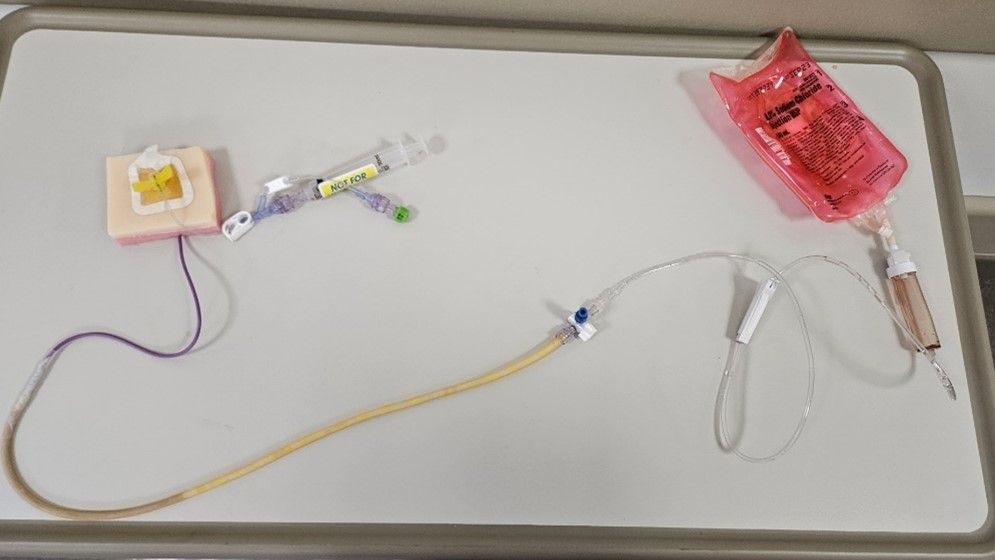
The port was then placed on manikin, accessed and dressed. In order to keep the dressing intact with the skin, some of the pink foam needed to be trimmed. This image shows the entire set-up.
View the LEARN CE/CME Platform Webinar Professional Development for Healthcare Simulation Operations Specialists to learn more!
For Blood Return
When thinking about obtaining blood return without diluting the blood supply first think about how a primary and secondary infusion work. Primary infusions are continuous over time, while the secondary line, which is higher on an IV pole, will intermittently infuse. This works through Fick’s first law of diffusion. Particles from a higher concentration will flow to a lower concentration to equalize (Knapp, 2021).
The drainage bag and blood bag were originally placed next to each other, which did not allow for an equal transfer. Also, due to the length of the tubing from port to blood, it didn’t facilitate ease of blood access without getting too dilute. By placing the drain bag lower and the blood access higher, allowed for the blood to be easily aspirated. When flushed, the pressure of the saline pushed to the lower concentration. Do note that due to gravity and the law of diffusion, when the blood supply is “running” it will continuously drain unless aspirating it back. In this scenario a 100mL bag was used as it could easily be tucked in a manikin’s sports bra or under their skin. The drainage bag was tucked in the manikin’s pants, or could be hidden in a pillowcase. The pictures below demonstrate this. It also shows where the 3-way stopcock was placed as compared to the original model without blood drawback.
What was tried and did not work?
Some materials were tried without success. If you do not first succeed, try and try again. Here are some items that did not work: Strategic Operations pleural skins, foam from C-Collar brace, and Gorilla Glue
The skins from the Strategic Operations kit gave a realistic feel and depth with the port but unfortunately the hospital’s port dressings would not adhere. The foam, when dried with the glue made the subcutaneous texture stiff and had random open gaps. If trialing again, the simulationists could attempt cutting the pleural skins down so the port dressing could surround the task trainer.
When thinking about obtaining blood return without diluting the blood supply the simulationist first thought about how a primary and secondary infusion work. Primary infusions are continuous over time, while the secondary line, which is higher on an IV pole, will intermittently infuse. This works through Fick’s first law of diffusion. Particles from a higher concentration will flow to a lower concentration to equalize (Knapp, 2021).
The drainage bag and blood bag were originally placed next to each other, which did not allow for an equal transfer. Also, due to the length of the tubing from port to blood, the ease of blood access was not facilitated without getting too dilute. By placing the drain bag lower and the blood access higher, allowed for the blood to be easily aspirated. When flushed, the pressure of the saline pushed to the lower concentration. Due to the Law of Diffusion, when the blood supply is “running”, this will continuously drain unless aspirating back. In this scenario, a 100 mL bag was used and easily tucked in the CAE Juno manikin’s sports bra. All lines can be tucked in the manikin’s pants. To allow for easier access to titration when simulation begins, the bolld line can be kept out. Blood supply can be tucked in manikin’s bra
Once completed, this port is not only a great training device for nurses and other staff on accessing ports, but this also can have an initial blood return and run fluids without leaks. This MediPort task trainer can be used on manikins and potentially on simulated participants. If this is used by a simulated participant, additional safety measures need to be taken to prevent an accidental needle stick. Kevlar, or another impenetrable backing would need to be placed behind the trainer to prevent accidental needle sticks.
Learn More About Using Task Trainers to Achieve Learning Outcomes
Reference
- Knapp, S. (2021, January 22). Osmolarity – the definitive guide. Biology Dictionary. https://biologydictionary.net/osmolarity/








