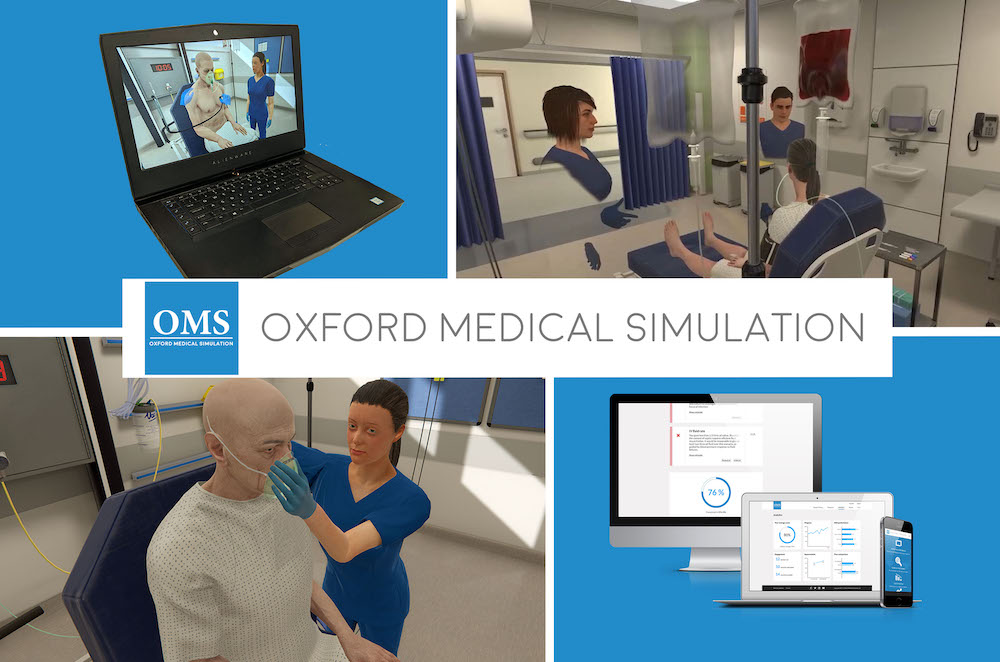
Oxford Medical Simulation (OMS) designs, builds, and delivers immersive experiential learning opportunities for healthcare students and practitioners. OMS offers learners access to over 240 clinical healthcare scenarios both in headset and on-screen. These scenarios can be run in person with supervision, or learners can remotely work through clinical simulations at their own pace, any time or anywhere. This HealthySimulation.com article will explore how Oxford Medical Simulation’s platform supports debriefing from VR scenarios.
Why Debriefing Extends Simulated Learning in Healthcare
Simulation-based education allows learners to apply their knowledge to clinical practice and assess their skill development. While a substantial amount of learning occurs during the simulation itself, the learning that happens afterward is equally crucial. Done well, debriefing is a time to engage in reflective thinking, process emotions, and gain a deeper understanding of clinical performance. According to the Society for Simulation in Healthcare (SSH) Dictionary (Lioce et al, 202, pg. 13), debrief is defined, as “to conduct a session after a simulation event where educators/instructors/facilitators and learners re-examine the simulation experience for the purpose of moving toward assimilation and accommodation of learning to future situations (Johnson-Russell & Bailey, 2010; National League for Nursing – Simulation Innovation Resource Center, 2013); debriefing should foster the development of clinical judgment and critical thinking skills (Johnson-Russell & Bailey, 2010). Debriefing works alongside deliberate practice, so learners can review their own work and take those lessons with them going forward.
Orientation and Prebriefing: Crucial to Success
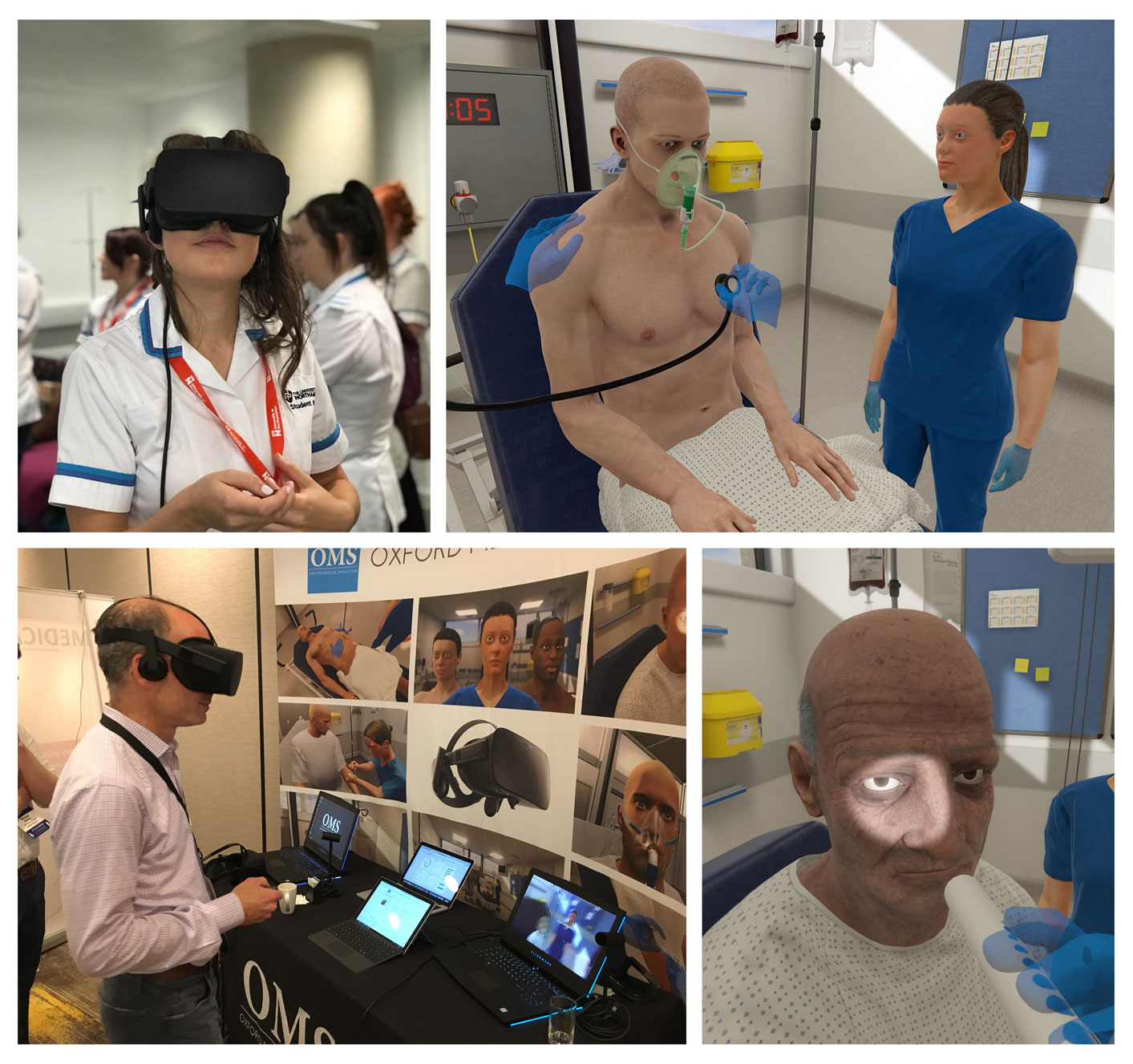
As the debrief serves a specific purpose, the prebrief plays an important role, too. For VR, prebriefing is crucial for learners to feel comfortable with the technology and for educators to feel capable of assisting learners, whether in a VR headset or on a desktop. Plenty of learners feel completely at ease in using technology like virtual reality, and plenty of others have yet to experience the technology with ease. Providing a comprehensive orientation and pre-brief gets everyone on the same page at the start.
Just as you would in any prebriefing, the facilitator must outline expectations, learning objectives, roles, and logistics of the experience. With OMS VR scenarios, an additional component may include having learners complete a walkthrough tutorial or related VR simulation ahead of time. Another route might be to provide a video showcasing the virtual environment. You may also open up access to a desktop-based simulation ahead of time, allowing learners to deliberately practice at their own pace in preparation for their VR experience.
Consider incorporating a room orientation in your prebriefing materials, so learners can get familiar with the environment. Learners can walk away with an understanding of where they can find equipment or review a chart, and how to navigate through the simulation at a high level. This can dispel anxieties around the unknown, opening up learners’ minds to focus on applying their skills rather than navigating an unknown environment.
View the LEARN CE/CME Platform Webinar Immersive Learning: Integrating VR Simulation and Continuity of Care in Nursing Education to learn more!
Debriefing After VR: An Additional Advantage for Learners
Following the completion of a scenario, learners should have time to reflect and discuss their experiences, whether on an individual or group basis. Depending on the chosen framework, many debriefing sessions include opportunities to reflect, process, ask questions, and discuss key takeaways.
Within the OMS platform, learners can receive immediate, objective feedback that includes rationale tied to competencies, as well as data around actions taken in the scenario. Learners get the chance to reflect on their clinical performance with their personal feedback before discussing with their peers or facilitator. Due to the immersive and realistic nature of OMS scenarios, certain situations like de-escalation or breaking bad news may warrant additional time to process emotions before digging into details of skill application.
In this phase, often referred to as the ‘reactive phase’, learners can explore their feelings related to the context of the scenario, patient outcomes, their own clinical performance, or with their skills. As learners are able to process and work through their emotional experience, they can progress to the analysis phase, going deeper into how their skills aligned with the learning objectives, any mistakes they made, and reflecting on the impact their decisions and actions had on patient outcomes.
Finally, learners can discuss the overall picture, pinpointing key takeaways they will use in their practice going forward. The OMS platform can complement all of this debriefing by providing individual or team-based feedback. This can decrease the facilitator’s cognitive load by keeping timestamps of actions taken and providing immediate feedback on performance.
From there, the facilitator can look at individual or group data, picking out trends or key features that would optimize debriefing discussions. Having access to real-time data can optimize debriefing discussions for educators and learners. Learners get a chance to reflect with personal feedback, while facilitators can focus on deeper insights rather than keeping track of all the learners’ actions.
OMS Platform and Debriefing VR Scenarios
Debriefing is arguably one of the most critical components of a simulation. Maintaining a safe learning space while providing appropriate feedback is crucial for learners to get the most out of the experience. OMS can be the solution to your simulation needs on a VR platform. To learn more about how the OMS platform can complement your debrief, stop by Booth 101 at INACSL to get the conversation started or book a demo with an Educational Specialist.
Learn More About the Oxford Medical Simulation (OMS) Virtual Platform and Debriefing!
References:
- Lioce L. (Ed.), Lopreiato J. (Founding Ed.), Downing D., Chang T.P., Robertson J.M., Anderson M., Diaz D.A., and Spain A.E. (Assoc. Eds.) and the Terminology and Concepts Working Group (2020), Healthcare Simulation Dictionary –Second Edition. Rockville, MD: Agency for Healthcare Research and Quality; September 2020. AHRQ Publication No. 20-0019. DOI: https://doi.org/10.23970/simulationv2.