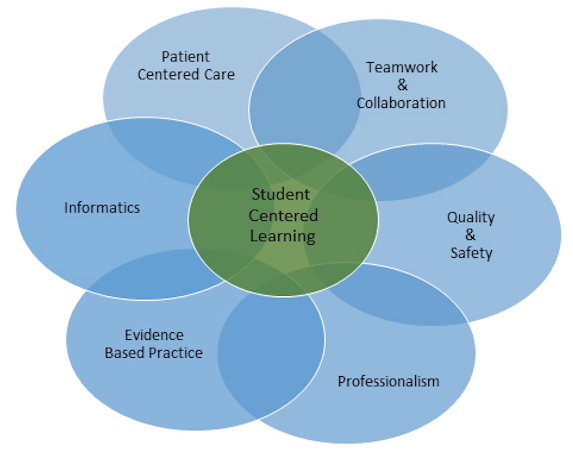
The Quality and Safety Education for Nurses (QSEN) project was designed to ensure that future nurses will have the knowledge, skills and attitudes (KSAs) necessary to continuously improve the quality and safety of the healthcare systems within which they work. Today guest author Dr. Kim Baily PhD, MSN, RN, CNE, shares about the six quality and safety competencies were developed for pre-licensure programs for QSEN and provides a template below for Debriefing them in Nursing Simulation experiences. Some Schools of Nursing use the QSEN competencies as part of their program or course outcomes.
Debriefing with QSEN competencies in mind helps students organize their reflection during debriefing in a systematic way. The list below offers numerous ways that that QSEN standards may be considered during scenario debriefing. Some standards are easier to incorporate into debriefing discussions than others. Select items from the list below to match the scenario content, level of student and healthcare professions participating in the scenario. Create checklists for debriefing with relevant items or create cues for students who are not participating in a scenario but observing. One option is to give each observing student a different QSEN standard to track during the scenario.
Safety: Minimizes risk of harm to patients and providers through both system effectiveness and individual performance. Include deliberate errors in scenario. Create errors that would require reporting e.g. IVPB hanging with incorrect patient identification or late administration.
- Assess patient, equipment and room for potential safety issues.
- Tag or remove defective equipment.
- Report potential or actual safety concerns.
- Identify national patient safety standards.
- Use appropriate checklists.
- Environment Check:
- Patient’s call light is within reach
- Clear pathways
- Bedside table within reach
- Bed lowered
- Bed rails – as needed
- Tubing Check.
- Trace ALL tubes from pumps, gas supplies and vacuums for appropriate connections to patient.
- Expiration dates.
- Maintenance IVs
- IV piggybacks.
- Clean linens
- Fluid containers covered with lids
- Medication Administration:
- Follow hospital policy for medication administration.
- Eight Rights of Medication
- Right patient (NBA- Name, Birthday, & Allergies)
- Right medication
- Right dose
- Right route
- Right time
- Right reason
- Right documentation
- Right response
- Infection Control
- Handwashing
- Appropriate glove use
- Appropriate disposal of contaminated items
- Touching hair face or glasses
- Cleaning diagnostic tools e.g. cleaning stethoscope.
- Complete incident report/discuss system processes for preventing errors.
- Use and identify safe practices to prevent injury to self.
Patient Centered Care: Recognize the patient or designee as the source of control and full partner in providing compassionate and coordinated care based on respect for patient’s preferences, values, and needs. Include items from the list below in scenarios. For example, include patients who refuse medications because of fear of side effects or lack of understanding of therapeutic effects. Another example is to have a confederate be a family member or friend at the bedside who should not have access to patient information. Finally have a patient whose religious beliefs are against blood transfusions and the physician has just ordered two units of blood.
- Determine the patient’s view of illness, beliefs and values as appropriate.
- Involve the patient in decision-making processes.
- Involve the patient when formulating a plan of care.
- Involve family members in the patient’s care.
- Ensure that information shared with family members does not breach patient confidentiality.
- Ensure plan of care is appropriate for the patient’s age, gender, and cultural and religious background.
- Value the patient’s expertise with their own health and symptoms.
- Value the range of human diversity and try to learn from the patient.
- Determine the patient’s pain and preferred methods for relieving pain.
- Communicate therapeutically with patient and family.
- Use terminology patient and family will understand.
- Use empathy to discuss embarrassing medical conditions.
- Complete patient assessment which is appropriate for the diagnosis or problem (assessment can be used as a separate topic).
- Convey patient’s wishes to other health care members.
- If appropriate to the scenario, determine the patient’s/family’s spiritual beliefs and ensure patient has access to spiritual support.
Teamwork and Collaboration: Function effectively within nursing and inter-professional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care.
- Appropriate delegation to auxiliary staff
- LVNs
- CNAs
- Help and support other nurses and staff members.
- Practice within own scope of practice.
- Request information from other team members when needed.
- Ask for help when needed.
- Identification of failure to speak up by a member of a team.
- Provide clear, relevant directions to all staff members.
- Complete accurate and concise SBAR (Situation, Background, Assessment, Recommendation) when communicating with all other staff including:
- Interdisciplinary staff members- pharmacists, PT/OT, Respiratory Therapists, MDs
- Assume role of team leader when appropriate.
Quality Improvement (QI): Use data to monitor the outcomes of care processes and use improvement methods to design and test changes to continuously improve the quality and safety of health care systems. To date, simulation has mostly been used as a learning strategy to help individuals or teams improve practice in given clinical situations. Simulation is however, an ideal research methodology for improving overall patient care. For example, in a mock code scenario, the observed behaviors of participants can be used to revise policies and procedures for the institution as a whole. Potential harmful situations/activities/equipment can be identified and changes made to existing policies.
- Identify gaps between local and best practice.
- Identify the effects of changes in practice/equipment/environmental design.
- E.g. relabeling or reshaping medication packaging to prevent errors.
- Test quality measures as useful and relevant tools.
- Identifying team behaviors/communication that could be improved.
- E.g. protocols for informing pharmacy about medication preparation or administration.
- Identifying interdisciplinary situations that might lead to errors.
Informatics: Use information and technology to communicate, manage knowledge, mitigate error, and support decision making. To some extent incorporation of informatics into scenarios will depend on the use of electronic health records (EHR) during the simulation.
- Retrieve relevant data from the EHR. E.g.:
- Potassium levels before administration of Lasix
- Dose of last PRN medication
- Previous response to blood pressure medications.
- Diagnostics.
- Identify clinical data that was not available but would have been helpful in making decisions about planned interventions.
- Evaluate patient response to interventions using informatics.
Evidence Based Practice: Integrate best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care.
- This QSEN competency is often more difficult to incorporate into a simulation exercise because of time limitations.
- Undergraduate learners can be assigned a prebriefing exercise to research current best practice prior to simulation.
- During debriefing compare learner performance to current best practice.
- Compare behaviors against course textbook/checkoff sheets and/or local hospital policies and procedures.
- Identify possible reasons for differences between references.
- Identify methods for learners to stay up to date in the future.
- For staff nurses and faculty, complete scenario and then debrief with current best practice i.e. identify practice gaps.
DOWNLOAD THE QSEN TEMPLATE HERE!
The use of QSEN competencies provides a systematic framework for debriefing. The QSEN standards help learners focus on the quality and safety of patient care not only on an individual basis but also as part of the larger healthcare system. In addition, Nursing programs that incorporate QSEN competencies into their course or program outcomes can show accreditors that the use of the QSEN competencies in simulation (and in the hospital setting) helps learners meet program outcomes.
Learn more about QSEN on their website!
Today’s article was guest authored by Kim Baily PhD, MSN, RN, CNE, previous Simulation Coordinator for Los Angeles Harbor College and Director of Nursing for El Camino College. Over the past 16 years Kim has developed and implemented several college simulation programs and previously chaired the Southern California Simulation Collaborative.
Have a story to share with the global healthcare simulation community? Submit your simulation news and resources here!