In a previous HealthySim article published April of 2018, Evidence-Based Practice (EBP) Defined for Simulation in Healthcare, EBP was defined and the difference between EBP and research was discussed. According to Burns and Grove 2007, “Evidence-based practice is the conscientious integration of best research evidence with clinical expertise and patients values and needs in the delivery of high quality cost-effective health care systems” (Burns, N and Grove, S.K. 2007. Discovering Nursing Research Understanding Nursing Research: Building an Evidence-based Practice. 4th Edition. Saunders).
Understanding research and its use in guiding EBP is not only important for ensuring that patients receive the best possible care, but also for finding and implementing the best simulation methodologies. In the early part of this century there was little research to support the use of medical simulation as an effective educational tool, however in the past fifteen years or so, extensive research has clearly revealed the benefits of simulation. In addition, medical simulation is being used to research new procedures, protocols and equipment before patients are exposed to potentially harmful interventions. Simulation team members need to understand research principals so that they can evaluate current research data and thus make informed decisions about the use of new clinical simulation methodologies.
The Scientific Process
Sim operations specialists use the Scientific Process on a regular basis. For example, one morning the manikin is turned on but nothing happens. An observation is made that the manikin is not working. A hypothesis or suggestion as to why the manikin is not working is made. An example might be that the battery of the wireless manikin needs charging. If the hypothesis is correct, when the battery is charged, the manikin should come to life. The hypothesis is tested to see if it is correct and the battery is plugged into the mains and allowed to charge. If the manikin now works, the hypothesis was correct but if it does not work the hypothesis was either wrong or the testing methodology did not accurately test the hypothesis. Other hypothesis might be that the battery is no longer accepting a charge, a lab breaker has been tripped, there has been a power failure or worse still the manikin is broken. Each one of these hypotheses could be tested with appropriate “research” until a reason for the manikin malfunction has been identified. Obviously, this is a very simple example of the use of the scientific method but the method itself forms the basis of scientific research as we know it today. Researchers often start off with the simplest, easily tested hypothesis and then test more complicated hypotheses. Why dismantle the manikin to see if manikin is broken, when a simple charge or breaker trip might solve the problem.
The Scientific Process in more detail, a breakdown:
- Conceptual Phase:
- Make an observation. For example:
- First semester nursing students frequently have difficulty giving shift reports.
- The survival rates for patients coding in the ER is below national levels. Observed codes seem chaotic.
- Simulation activities improve student learning.
- Examine the clinical/educational influences. For example:
- Content covered in class.
- Skills lab practice with SBAR/shift report
- Acuity of patients admitted to ER
- Staffing ratios
- Current training practices and standards.
- Literature review:
- Research already conducted on similar or same issue.
- Develop a research question
- Why do students have a hard time giving a shift report?
- Why are ED outcomes lower than national standards?
- Which debriefing methods produces the greatest learning?
- Formulate a hypothesis
- A hypothesis is an assumption, an idea that is proposed for the sake of argument so that it can be tested to see if it might be true. In the scientific method, the hypothesis is constructed before any applicable research has been done, apart from a basic background review (Merriam Webster). For example:
- If simulation time increases, student communication ability will increase.
- If ER staff practice team communication strategies in simulation, code outcomes will improve.
- If students participate in instructor led debriefing, their learning will increase more than if they self-debrief.
- The hypothesis must be able to be tested by some kind of experiment or by data collection of some kind.
- Identify the dependent variable: the variable being measured in the experiment e.g. student communication, code outcomes.
- Identify the independent variable: a variable whose variation does not depend on that of another E.g. time spent in simulation, participation in a particular type of experience (often designated the y variable).
- A hypothesis is an assumption, an idea that is proposed for the sake of argument so that it can be tested to see if it might be true. In the scientific method, the hypothesis is constructed before any applicable research has been done, apart from a basic background review (Merriam Webster). For example:
- Make an observation. For example:
- Planning Phase
- Testing hypotheses means there will be some kind of data collection.
- How will data be measured?
- What specific criteria will be used?
- In the example above, how will student communication be measured.
- Will a questionnaire be developed (aka a data collection instrument)?
- This may seem like an easy task to accomplish but it is often complex. An instrument must provide data which will answer the hypothesis exactly.
- How will nursing student communication skills be measured?
- Using an existing instrument that has already been tried and tested can save a huge amount of time.
- This may seem like an easy task to accomplish but it is often complex. An instrument must provide data which will answer the hypothesis exactly.
- Identify the population to be followed.
- E.g. first semester students in specified week of course.
- E.g. ED patients with specified admit criteria.
- Will there be an experimental control group?
- A control group that does not receive any intervention compared to a group that receives an intervention e.g. as in drug testing.
- Sometimes experiments cannot be conducted for ethical reasons but existing data may be used to confirm a hypothesis. For example, the hypothesis that increased BMI in teenagers leads to an increase in Type 2 diabetes in early adulthood can be tested by using population studies which compare BMI with diabetes rates to see if there is any relationship between the two.
- Develop protocols that will ensure data collection will be consistent between subjects and research staff.
- Define the variables.
- Internal Review Board approval to protect patient or student rights.
- Single blind or double blind study.
- Single-blind: The subject does not know which intervention is being used, but the researcher does.
- Double-blind: Often used in drug research when neither the subject or researcher know if the medication given is a placebo or the test drug.
- Determine the time needed for data collection, analysis and publication.
- Data Collection
- Collection instrument.
- Chart review.
- Interviews.
- Surveys.
- Direct observation.
- Analysis Phase
- Quantitative – use of statistics
- Qualitative – content analysis
- Interpretation of findings
- Significant versus nonsignificant
- Unexpected findings
- Clinical significance
- Recommendations
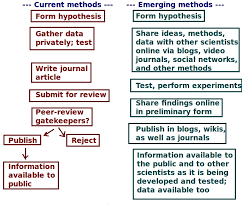
- Dissemination Phase
- Publication
- Journal submission
- Conference presentation.
- Publication
Evidence-based practice should now drive patient care and simulation and, since EBP is based on sound research, understanding the research process should enable simulation technicians, educators and administrators to engage more fully in simulation development.
Understanding Research for Clinical Simulation Series:
-
- Part 1: The Scientific Process
- Part 2: Validity and Reliability
- Part 3: Statistics
- Part 4: P Values
Today’s article was guest authored by Kim Baily PhD, MSN, RN, CNE, Simulation Coordinator for Los Angeles Harbor College. Over the past 15 years Kim has developed and implemented several college simulation programs and currently chairs the Southern California Simulation Collaborative.
Have a story to share with the global healthcare simulation community? Submit your simulation news and resources here!








